This study was published on Research Square as a preprint and has not yet been peer reviewed.
Key Takeaway
-
Patients with HER2-positive breast cancer whose first metastatic event is an isolated brain lesion have worse overall survival than patients with concurrent extracranial disease (ECD) who develop brain metastases later in their metastatic course.
Why This Matters
-
Current first-line systemic therapies for advanced HER2-positive breast cancer, including pertuzumab and trastuzumab, control metastases outside of the central nervous system, but do not readily cross the blood–brain barrier and can allow for metastatic escape into the central nervous system.
-
The finding of worse overall survival with isolated brain metastases highlights the need for more agents that are effective against both intracranial and extracranial lesions.
-
The investigators said that clinical trials of HER2-targeted therapies that can cross the blood–brain barrier, such as the oral tyrosine kinase inhibitor tucatinib (Tukysa), are warranted.
Study Design
-
The team at Duke University assessed survival outcomes in 153 patients with HER2-positive breast cancer who presented with their first metastatic brain lesion from 2008-2020.
-
Almost three quarters had concurrent ECD — defined as any metastasis outside of the brain — at diagnosis, the majority with stable/responding ECD and the rest with progressive disease.
-
The remaining 27% presented with isolated intracranial relapse or no evidence of concurrent ECD.
-
After radiation, 23% of patients were treated with HER2-targeted trastuzumab (Herceptin) and pertuzumab (Perjeta), 19% with trastuzumab but not pertuzumab, 19% with lapatinib (Tykerb), and 15% with ado-trastuzumab emtansine based therapy.
Key Results
-
Overall survival from initial metastatic disease to death was 28.4 months for patients with isolated brain metastases vs 48.8 months for those with concurrent progressive ECD and 68.1 months with stable/responding ECD (P = .0035).
-
Overall survival from radiation to death was significantly worse for patients with progressive ECD (17.8 months) vs isolated intracranial relapse (28.4 months) and stable/responding ECD (36.6 months).
-
There was no statistically significant difference in intracranial progression-free survival based on ECD status.
Limitations
-
This was a single-institution, retrospective study with a range of possible confounders.
-
Few patients were treated with newer HER2-targeted agents such as trastuzumab deruxtecan and tucatinib.
Disclosures
-
The work was funded by the Duke University Department of Medicine.
-
Investigators reported numerous industry ties, including to SeaGen/Seattle Genetics, maker of tucatinib.
This is a summary of a preprint research study, “Brain metastasis as the first and only metastatic relapse site portends worse survival in patients with advanced HER2+ breast cancer,” led by Laura Noteware, BASc, of Duke University. The study has not been peer reviewed. The full text can be found at researchsquare.com.
M. Alexander Otto is a physician assistant with a master’s degree in medical science and a journalism degree from Newhouse. He is an award-winning medical journalist who has worked for several major news outlets before joining Medscape and also an MIT Knight Science Journalism fellow. Email: aotto@mdedge.com.
For more news, follow Medscape on Facebook, Twitter, Instagram, YouTube, and LinkedIn
Credits:
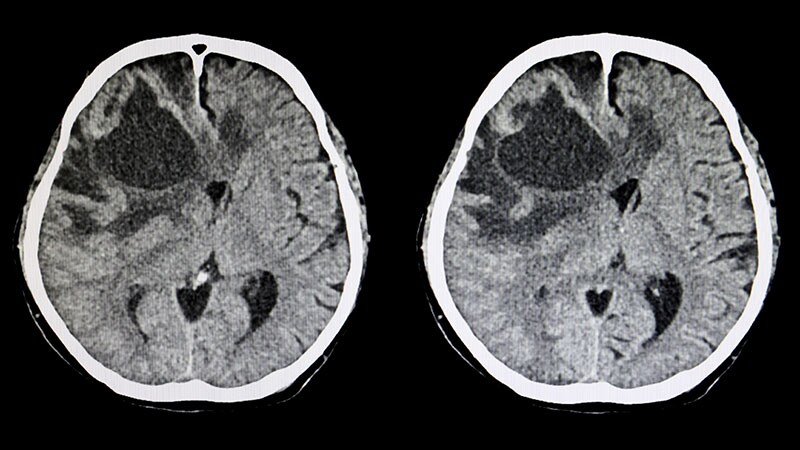
Lead Image: Sopone Nawoot/Getty Images
© 2022 WebMD, LLC
Send news tips to news@medscape.net.
Cite this: Much Worse Breast Cancer Survival When First Metastasis in Brain - Medscape - Aug 29, 2022.