New cancer treatment that tracks and zaps tumors is coming to Stanford Medicine
A new technology aims to make tumors their own worst enemy in the fight
against cancer — and Stanford Medicine will be the first in the world to
incorporate the treatment into the clinic.
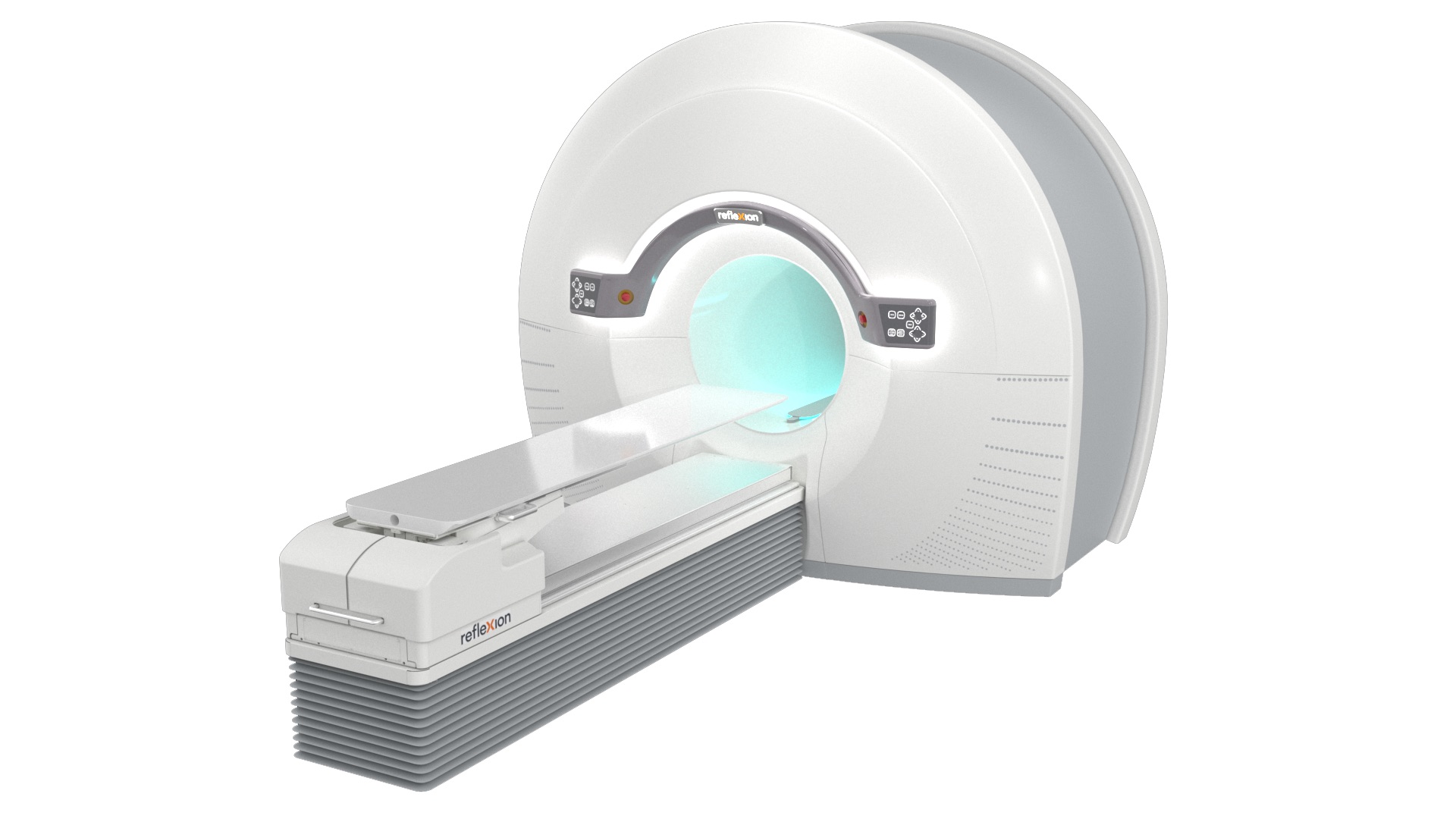
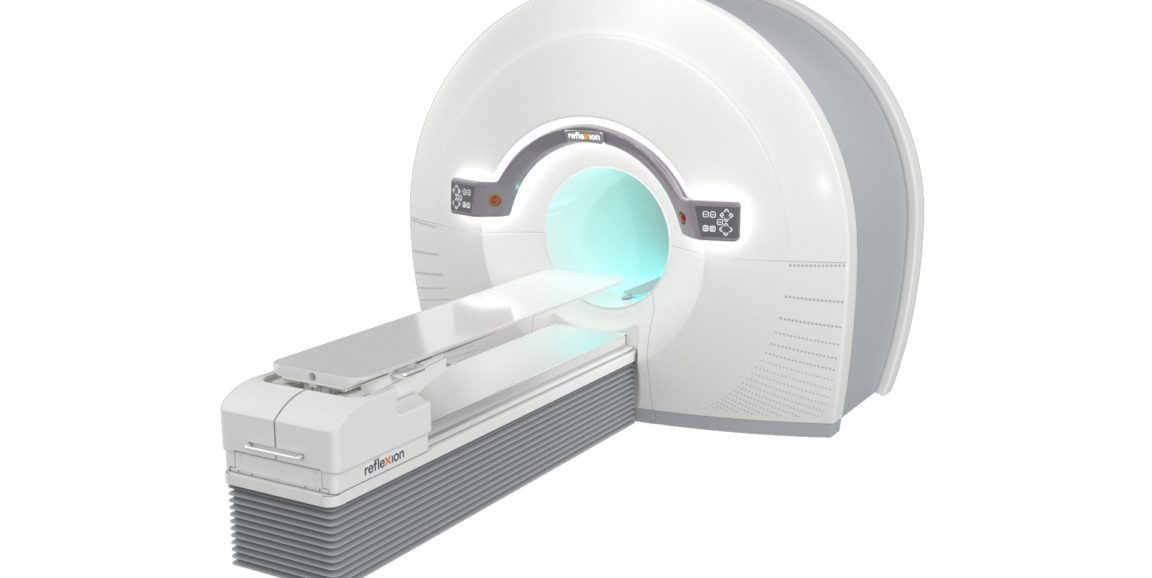
The first generation of a machine using this technology – the X1, from
the company RefleXion Medical — harnesses positron emission tomography to deliver
radiation that tracks a tumor in real time. This PET feedback allows the system
to send beams of radiation to destroy cancerous cells with heightened
precision.
Researchers hope that this “biology-guided radiotherapy” will increase accuracy, safety and efficacy of cancer radiation treatment. Stanford physicians plan to test the X1 later this year through clinical trials at Stanford Hospital. Their first step will be to obtain approval by the Food and Drug Administration.
“To my knowledge, this machine is the first of its kind. It combines
two technologies – one traditionally
used in cancer diagnostics, and one in therapeutics — into a single
technology,” said Daniel
Chang, MD, professor of radiation oncology, who will lead the clinical
trial. “That’s what makes this really unique.”
Radiation therapy is often one of the primary tools used to treat cancer.
But the therapy, which bombards tumors with high-energy particles that kill
cancer cells, comes with a downside: The beam of destructive particles does not
discriminate between cancerous and non-cancerous cells, and healthy cells are
often damaged in the line of fire.
With this new technology, the PET scanner provides continuous feedback about
the location of a tumor, based on the tumor’s emissions, even if the tumor
moves as a patient breathes. This PET feedback allows doctors to continue
training beams of radiation on cancerous cells, even as the tumor’s location
shifts. With less risk of targeting healthy cells, doctors would be better able
to zero in on tumors with higher doses of radiation, executing more accurate
and precise radiation therapy, Chang said.
Samuel Mazin, PhD, co-founder and chief technology officer of RefleXion Medical, thought up the idea for the new technology while he was a Stanford postdoctoral scholar. Stanford Medicine will be the first to conduct clinical trials with the new machine. Both components of the machine — PET scans and radiation — have well-established safety profiles.
Chang and his colleagues hope that the technology will help open new avenues
of research, such as clinical trials for patients with multiple tumors who may
otherwise not be eligible for radiation therapy. The technology also could lead
to studies to develop novel and more sensitive PET tracers — molecules that
reveal where cancer is in the body — to assess the inherent biology of tumors
and their response to treatment.
“We’re excited about this technology for many reasons,” Chang said. “It
opens up new possibilities for treatment by allowing us to deliver radiation
that tracks the tumor with extreme precision in real time — something we’re not
currently able to do.”
Photo courtesy of RefleXion ©2020. All rights reserved.
Popular posts
Category:

How viruses like the coronavirus can steal our sense of smell
Category:
What’s a virus, anyway? Part 1: The bare-bones basics