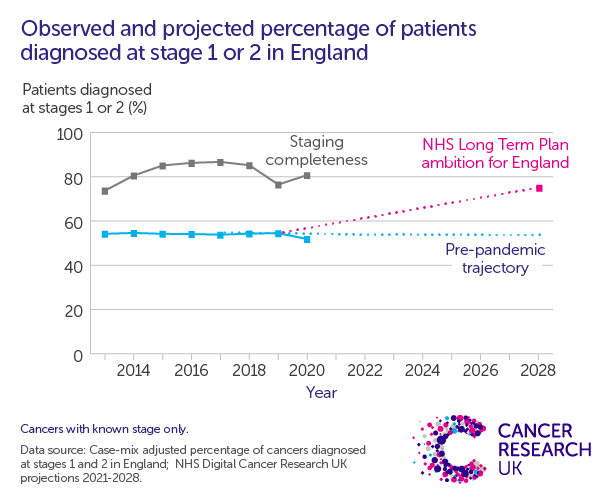
One of the best ways to help people survive cancer is to find it early. That’s why NHS England has a target of diagnosing 75% of cancer cases in stage 1 or 2 by 2028.
Unfortunately – despite the tireless work of NHS staff, as well as a range of national strategies and initiatives – it looks like we’re going to fall well short of that target. The proportion of people diagnosed early had been stuck at around 54% since 2013. In 2019, it was already clear that we needed to do more, and that we needed the right workforce and equipment to make progress. And then COVID-19 happened.
The pandemic disrupted cancer services and changed people’s behaviours. In England, screening programmes were effectively paused for several months, far fewer people visited the doctor for cancer symptoms and services struggled with increased restrictions and reduced capacity.
And one question we’ve been asked regularly over the last couple of years is: how has the pandemic affected early diagnosis?
Research from earlier in the pandemic tried to model its impact, but the evidence was very limited.
Now, though, we have good quality data for 2020, which means we can begin to answer the question.
But, while we’d love to be able to give you a definitive account of how COVID-19 impacted early diagnosis, it’s a complex, cloudy picture and we still don’t have all the answers.
Even so, what we do know is important, and it needs to be explained.
Numbers vs proportions
In 2020 in England, the proportion of people diagnosed early was 52%, a drop from previous years and putting the 75% ambition even further out of reach. This is definitely a setback.
But looking at the number of people behind this proportion tells an even more concerning story.
Around 27,500 fewer people were diagnosed with cancer in 2020 compared to previous years.[1] That reduction was spread across almost all cancer sites, with drops driven by pauses in screening programmes, worry about COVID-19 and messages to stay home, as well as increased pressure on cancer services.
Our analysis suggests these ‘missing’ cases were disproportionately early-stage ones – we estimate around 72% of them.[2] The impact of the pandemic on early diagnosis now looks even more worrying.
Are these cases “missing”?
We’ve seen multiple articles about finding these cancer cases as soon as possible – clearing the ‘backlog’, so to speak.
For some of the people these cases represent, that makes sense. Screening programmes have been working hard to restore services, sending out invitations to those who may have missed appointments. Meanwhile, more and more people are seeing their doctor with symptoms they are worried about. But we’re concerned that some of these patients may have presented later than they would have otherwise, with more advanced disease. It’s not possible to simply clear the backlog of missed diagnoses because cancer develops over time.
Also, not all these cases are ‘missing’. Sadly, some of these people will have died before their cancer diagnosis, many from COVID-19, which means we’ll never diagnose or treat them.
Known unknowns
The puzzle gets even more complicated when we consider cases of unknown stage.
These are cases where there isn’t enough information submitted about a person’s cancer when it gets recorded by the cancer registry to determine what stage it is. This might be because the information wasn’t collected in the first place, or because of a problem during the registration process.
It is normal to have some cancers with unknown stage – in previous years around 14% of cancers were missing staging information. But since the pandemic we’ve seen a 17% increase in these cases.
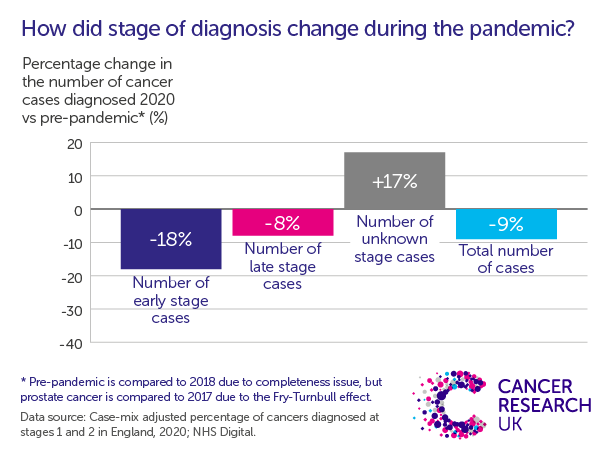
This increase means that we know less about the cancers that were diagnosed. It increases the uncertainty about whether any observed changes in early diagnosis (or lack of) are real, or whether the increase in unknowns is just obscuring the picture.
The combination of missing cases and the increase in the number of cases of unknown stage means we still can’t say for sure how the pandemic has affected early diagnosis.
There’s also more to survival than diagnosis at an early stage
We talk a lot about the importance of early diagnosis of cancer, and for good reason. Diagnosis at an early stage does give people with cancer the best chance of a good outcome.
But the impact of the pandemic won’t just be seen in changes in overall early diagnosis. We’re also concerned more generally about people being diagnosed later than they would have been, even if there is no difference to whether this means they are early or late stage.
This is because, for some types of cancer, smaller differences in stage can make a big difference to survival. Prostate cancer, one of the most common in the UK, is an important example. Around 95% of people diagnosed with the disease at stage 3 will survive for 5 years. That proportion drops down to 50% for people diagnosed at stage 4. These groups are both ‘late-stage’, but their outcomes look very different.
Delays to diagnosis or treatment can also have an effect on outcomes, even when we see no change in stage. Cancers may grow, or people may see declines in their general health and fitness while waiting for a diagnosis or treatment. In 2020, the general health of people diagnosed with lung cancer was lower compared to 2019.
All this together means that understanding the effects of the pandemic isn’t at all straightforward.
So what do we know?
We don’t need years of data to understand that the pandemic had a huge impact on people and the NHS.
We know that people with signs and symptoms of cancer stayed home and didn’t visit their GP. We know services saw big changes, like the switch to more remote appointments at GP surgeries or the pausing of screening programmes. And we know that difficult decisions had to be made about how best to deploy already stretched resources.
We’re still feeling the ramifications. Cancer waiting times, which measure how long people wait for diagnosis and treatment, are among the worst on record. Services were struggling to meet waiting times targets for many years before the pandemic, and declines in performance have accelerated drastically since it began. For example, in October 2022, less than 4 in 10 (38.2%) people diagnosed with lower gastrointestinal cancer started their treatment within 2 months of their urgent GP referral.[3]
Where do we go from here?
Ultimately, we need to see better outcomes for people affected by cancer.
Many of the long term effects of the pandemic on cancer services and disease outcomes are still unclear. We may never be able to fully disentangle its impact. But what we do know for certain that we already had a very long way to go.
After almost a decade of stubbornly stable early diagnosis rates, cancer waiting times and an increasingly stretched cancer workforce, it’s not hard to see the challenges that we need to tackle right now. Patients deserve better. In the short term, we need to get cancer services back on track by addressing the gap between NHS capacity and patient need – most notably by transforming services and investing in much-needed staff and equipment.
And, long term, if we are to improve cancer survival, we must go further to reduce late stage cancer diagnosis. That’ll need concerted action on all fronts to transform screening services, streamline diagnostic pathways, and get the benefits of innovation and research to patients more quickly.
The Government right now has a massive opportunity to do all that, through a comprehensive, funded, long term plan for cancer. If Prime Minister Rishi Sunak and Health Secretary Steve Barclay commit to this, as their predecessors did, we could truly take our cancer services from world lagging to world leading and give every cancer patient the outcomes they deserve.
Lyndsy Ambler, Senior Strategic Evidence Manager
Sophia Lowes, Senior Cancer Intelligence Manager
References
[1] 27,528 fewer ‘All Cancers Combined’ cases (including missing and unstageable) were diagnosed in 2020 when compared to a composite pre-pandemic baseline. For most sites, a 2018 baseline was selected due to a dip in staging completeness for 2019 data (76.5%) compared to previous years (85.3% in 2018). This is with the exception of prostate cancer which was compared to 2017 cases (due to unusually high incidence of prostate cancer diagnoses in 2018 from the ‘Fry and Turnbull effect’), and oropharyngeal cancer which was compared to 2019 cases (due to changes in TNM classification causing more tumours to be classified as ‘oropharyngeal cancer’ from 2019 onwards).
Data source: Case-mix adjusted percentage of cancers diagnosed at stages 1 and 2 in England, 2020; NHS Digital; https://digital.nhs.uk/data-and-information/publications/statistical/case-mix-adjusted-percentage-of-cancers-diagnosed-at-stages-1-and-2-in-england/2020
[2] The proportion of ‘missing’ cases diagnosed in early stage out of all ‘missing’ cases with a known stage. The difference in the number of people diagnosed in early stage and late stage in 2020 vs a composite pre-pandemic baseline creates a total number of ‘missing’ cases with a known stage. There were 24,627 missing early stage cases and 9,748 missing late stage cases.
Data source: Data source: Case-mix adjusted percentage of cancers diagnosed at stages 1 and 2 in England, 2020; NHS Digital; https://digital.nhs.uk/data-and-information/publications/statistical/case-mix-adjusted-percentage-of-cancers-diagnosed-at-stages-1-and-2-in-england/2020
[3] Data source: Cancer Waiting Times – Time Series, NHS England; https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/
