The coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pathogen, is a novel disease that scientists are racing to better understand. This has been in the hope of developing therapeutic and prophylactic approaches to help save lives and curb the virus’s spread.
A team of researchers at the Robert Wood Johnson Medical School, Rutgers University, USA, have investigated a case wherein a man experienced recurrent episodes of Guillain–Barré Syndrome after being infected with SARS-CoV-2.
Their study is available in the latest issue of the journal Pathogens (November 2020).
Guillain–Barré Syndrome (GBS) and COVID-19
Guillain–Barré Syndrome (GBS) is a rare disorder wherein the body’s immune system attacks the nerves. The common signs and symptoms of the condition include weakness and tingling in your extremities. As the condition worsens, the sensations quickly spread, eventually paralyzing the whole body.
Recent research has shown that COVID-19 has been tied to a wide range of immune neuropathies, including GBS. It has also been linked to the worsening of chronic inflammatory demyelinating polyradiculopathy (CIDP).
Recurrent GBS is defined as two or more GBS episodes with less than four months between episodes without full recovery, or more than two months between episodes if the patient exhibits complete or near-complete recovery.
Patient case
The case study highlights the case of a man who had recurrent GBS over the course of a few years. When he experienced his most recent bout due to COVID-19, his symptoms were worse.
The patient was a 43-year-old man who has been in a motor vehicle accident and came to the Rutgers Robert Wood Johnson University Hospital (RWJUH) Emergency Department with chief complaints of numbness and tingling in both his upper extremities. He also had a patchy sensory loss in his upper extremities.
The patient suffered other injuries in the cervical and lumbosacral spine and was diagnosed with a herniated disc. Four years later, the patient developed an acute illness with cough, fever, and ageusia, wherein food tasted like clay. He was eventually diagnosed with Influenza A.
However, three days after the first diagnosis, he developed numbness in both his arms and legs. Later, it progressed to his trunk. He had slurred speech and facial weakness, with diagnoses of GBS, multiple sclerosis, and Lyme disease. He completely recovered within one week without any treatment.
He had two more similar episodes after viral infections. In April 2020, the now 54-year-old patient presented to the emergency room with complaints of progressive difficulty swallowing. He had a fever for three days, followed by weakness on the arms, legs, and face.
The doctors conducted tests to determine the cause of his febrile episode, and the reverse transcription-polymerase chain reaction (RT-PCR) test for COVID-19 turned out positive. The doctors treated the patient for rGBS secondary to COVID-19.
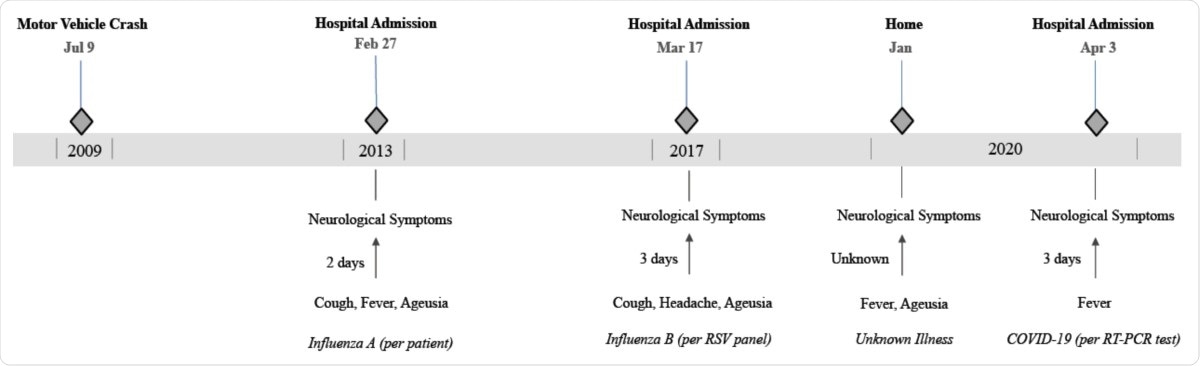
The patient described the GBS symptoms in his latest bout, triggered by COVID-19, presented with worse symptoms.
The researchers noted that this is the first case of recurrent GBS tied to COVID-19, showing that its severity was enhanced compared to past episodes.
“The growing body of research will likely show that the rate of GBS in COVID-19 patients is higher than the background GBS incidence. Studying rGBS patients allows us to understand COVID-19 pathophysiology better and for comparisons with other viral antecedents to GBS,” the researchers wrote in the paper.
“For patients who have a history of inflammatory demyelinating polyradiculopathies who develop COVID-19, we recommend close observation for neurologic symptoms over the next days and weeks,” they added.
The COVID-19 pandemic to date
COVID-19 is a novel viral disease that is wreaking havoc across the globe. To date, over 60.57 million people have been infected. Further, the virus has claimed more than 1.42 million lives. Many countries are reporting skyrocketing cases, including the United States, India, Brazil and France.
The United States has over 12.79 million confirmed cases and more than 262,000 deaths. India, Brazil and France follow a staggering 9.26 million, 6.16 million and 2.22 million cases.
The United Kingdom has reported a steep rise in COVID-19 cases in the past two months; the country has over 1.56 million cases and 57,000 deaths.
Mexico has seen a high death rate due to COVID-19. With over 1 million cases, the death toll there has reached a staggering 103,000.