Researchers in the UK have conducted a study assessing the efficacy of the Pfizer-BioNTech COVID-19 vaccine BNT162b2 against the new variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes coronavirus disease 2019 (COVID-19).
The new B.1.1.7 variant, which has higher transmission potential than previous SARS-CoV-2 strains, recently emerged in the UK, South Africa and Brazil and has now been identified in 50 countries.
The emergence of B.1.1.7 has triggered concerns over whether the vaccines that are currently being rolled out in an effort to control the COVID-19 pandemic will still be effective against SARS-CoV-2.
Now, Ravindra Gupta from the University of Cambridge and colleagues have demonstrated evidence of a reduced antibody response against the B.1.1.7 mutant among individuals (aged between 64 and 85) three weeks after they received the first dose of the Pfizer BioNTech vaccine BNT162b.
However, the researchers say the reductions were expected, that vaccines should still retain good activity and that vaccination is still a priority.
Nevertheless, “further work is needed to establish the impact of these observations on real-life vaccine efficacy,” adds the team.
A pre-print version of the research paper is available on the medRxiv* server, while the article undergoes peer review.
Vaccines have quickly emerged, but so have variants
Since the COVID-19 outbreak first began in Wuhan, China, in late 2019, the rapid spread of SARS-CoV-2 has culminated in a global pandemic that has had scientists racing to develop vaccines against the causative agent SARS-CoV-2.
The unprecedented scientific response to this global challenge has led to three vaccines now being licensed for use, namely the Pfizer BioNTech BNT162b2 vaccine, the Moderna mRNA-1273 vaccine, and the Oxford-AstraZeneca ChAdOx1 nCoV-19 vaccine.
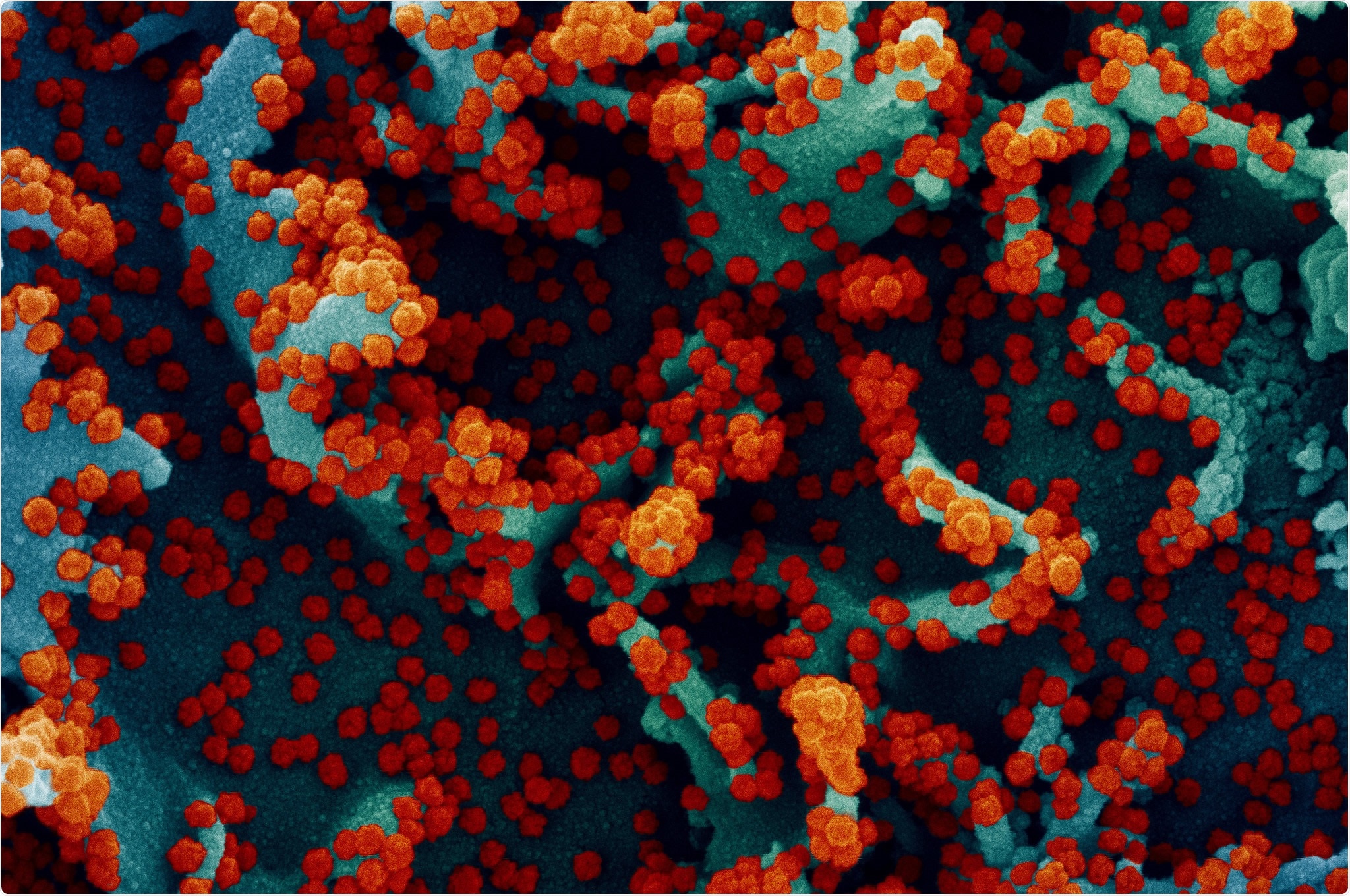
These vaccines all target a protein expressed on the surface of SARS-CoV-2 called spike, which is the main structure the virus uses to bind to and infect the cell.
However, these vaccines were designed against the Wuhan strain isolated in 2019. Since then, the virus has evolved to optimize its infectivity and evade being targeted by drugs and the immune system.
Now, SARS-CoV-2 transmission has been confounded in many areas of the world by the recently emerged B1.1.7 variant, which has now been identified in 50 countries.
Concerns are growing as to whether the Pfizer BioNTech, Moderna, and Oxford-AstraZeneca vaccines will be effective against this new variant.
Furthermore, vaccine supply is limited, and many governments have had to extend the interval time between first and second doses in order to expand vaccine coverage.
“Information on vaccine-elicited responses in real-world settings outside of highly selective clinical trials is important,” says Gupta and colleagues. “It is unclear whether real-world neutralizing antibody titers will follow those in clinical trials, particularly in elderly persons, and how this will be impacted by mutations in strains such as B1.1.7.”
What did the researchers do?
Gupta and colleagues assessed immune responses induced three weeks following one dose of the Pfizer BioNTech vaccine BNT162b2 vaccine among 23 individuals who have received the first dose as part of vaccine rollout in the UK.
The team also tested neutralizing antibody responses against pseudoviruses engineered to express wild-type spike protein or the three key mutations present in B.1.1.7 (deletion 69/70, N501Y, A570D). In addition, the team tested a panel of sera from eleven individuals who had recovered from SARS-CoV-2 infection.
The study cohort had a median age of over 80 (82 years), in line with the targeting of this age group in the initial UK vaccine rollout.
What did the study find?
The team reports that titers of anti-spike immunoglobulin G (IgG) correlated well with neutralization responses.
The data showed that ant-spike IgG antibody titers were much higher among vaccinated individuals than among healthy controls and were similar to those seen among recovered individuals.
However, there was an almost 100-fold variation in IgG responses among the vaccinated participants. Those older than 80 years exhibited significantly reduced IgG responses and lower neutralization potency than those younger than 80.
“This may or may not be compensated for by the second dose and it will be important to follow all participants over the following months for measurement of neutralization activity as well as data on re-infection,” say the researchers.
How did the three B.1.1.7 mutations affect immune responses?
The three B.1.1.7 mutations in spike did not significantly impact neutralization titers among recovered individuals or people who had been vaccinated.
Next, the team engineered a pseudovirus to express spike protein that included the full set of mutations present in the B.1.1.7 variant (del69/70, del 144/145, N501Y, A570D, P681H, T716I, S982A, D1118H).
When sera were tested against this full set of B.1.1.7 spike mutations, neutralization titers were reduced among the vaccinated individuals.
Among 15 individuals who had exhibited neutralization activity three weeks following vaccination, 10 showed evidence of a reduced antibody response against the B.1.1.7 mutant.
Overall, the reduction in efficacy was less than 3-fold, while the most significant reduction was around 6-fold, and the median reduction was 3.85-fold.
Vaccination remains a priority, but further research is needed
“These modest changes are what we expected to see given the mutational profiles. Vaccines should still retain good activity and vaccine coverage is a priority,” write the researchers.
However, further research is needed to investigate the impact of these observations on real-life vaccine efficacy, says Gupta and colleagues
“Other variants also need to be tested against vaccine sera, some with more concerning mutations such as E484K and K417N that have been shown to impact neutralization by monoclonal antibodies or convalescent sera,” concludes the team.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.