Patients with degenerative mitral valve (MV) regurgitation that calls for surgery may, for the most part, safely choose either a standard procedure requiring a midline sternotomy or one performed through a mini-thoracotomy, suggests a randomized comparison of the two techniques.
Still, the minimally invasive approach showed some advantages in the study. Patients’ quality of recovery was about the same with both procedures at 12 weeks, but those who had the minimally invasive thoracoscopy-guided surgery had shown greater improvement 6 weeks earlier.
Also in the UK Mini Mitral Trial, hospital length of stay (LOS) was significantly shorter for patients who underwent the mini-thoracotomy procedure, and that group spent fewer days in the hospital over the following months.
But neither procedure had an edge in terms of postoperative clinical risk in the study. Rates of clinical events, such as death or hospitalization for heart failure (HHF), were about the same over 1 year.
Patients in this trial had been deemed suitable for either of the two surgeries, which were always performed by surgeons specially chosen by the steering committee for their experience and expertise.
This first randomized head-to-head comparison of the two approaches in such patients should make both patients and clinicians more confident about choosing the minimally invasive surgery for degenerative MV disease, said Enoch Akowuah, MD, Newcastle University, United Kingdom.
Akowuah presented the UK Mini-Mitral Trial March 5 at the American College of Cardiology (ACC) Scientific Session/World Congress of Cardiology (WCC) 2023, held live and virtually from New Orleans, Louisiana.
The researchers assigned 330 patients with degenerative MV disease who were deemed suitable for either type of surgery to undergo the standard operation via sternotomy or the mini-thoracotomy procedure at 10 centers in the United Kingdom. The steering committee had hand-selected its 28 experienced surgeons, each of whom performed only one of the two surgeries consistently for the trial’s patients.
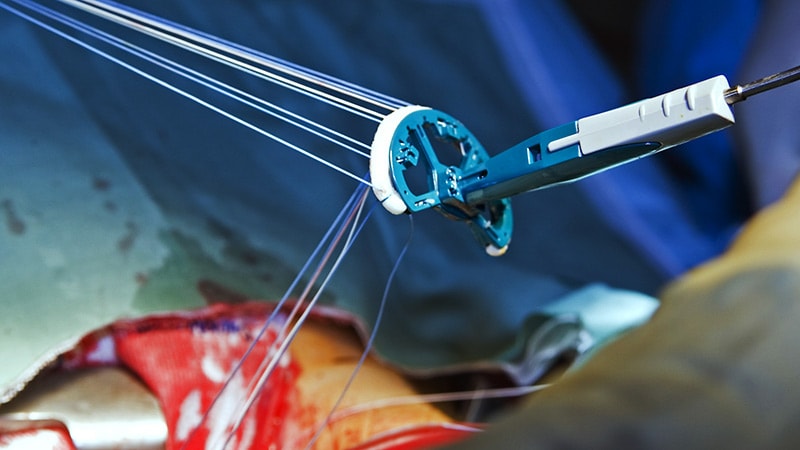
The technically more demanding mini-thoracotomy procedure took longer to perform by a mean of 44 minutes, it prolonged cross-clamp time by 11 minutes, and it required 30 minutes more cardiopulmonary bypass support, Akowuah reported.
The two patient groups showed no significant differences in the primary endpoint of physical function and ability to return to usual activity levels at 12 weeks, as assessed by scores on the 36-Item Short Form Survey (SF-36) and wrist-worn accelerometer monitoring. At 6 weeks, however, the mini-thoracotomy patients had shown a significant early but temporary advantage for those recovery measures.
The mini-thoracotomy group clearly fared better, however, on some secondary endpoints. For example, their median hospital LOS was 5 days, compared to 6 days for the sternotomy group (P = .003), and 33.1% of the mini-thoracotomy patients were discharged within 4 days of the surgery compared to only 15.3% of patients who had the standard procedure (P < .001).
The mini-thoracotomy group also had marginally more days alive out of the hospital at both 30 days (23.6 days vs 22.4 days in the sternotomy group) and 90 days (82.7 days and 80.5 days, respectively) after the surgery (P = .03 for both differences).
Safety outcomes at 12 weeks were similar, with no significant differences in rate of death, strokes, myocardial infarction, or renal impairment, or in intensive care unit length of stay or need for more than 48 hours of mechanical ventilation, Akowuah reported.
Safety outcomes at 1 year were also similar. Mortality by then was 2.4% for the mini-thoracotomy patients and 2.5% for the sternotomy group, nor were there significant differences in HHF rates or need for repeat MV surgical repair.
Akowuah said the patients will be followed for up to 5 years for the primary outcomes, echocardiographic changes, and clinical events.
The study was funded by the United Kingdom’s National Institute for Health and Care Research. Akowuah reports no relevant financial relationships with industry.
American College of Cardiology (ACC) Scientific Session/World Congress of Cardiology (WCC) 2023. Presented March 5, 2023.
Follow Steve Stiles on Twitter: @SteveStiles2. For more from theheart.org | Medscape Cardiology, follow us on Twitter and Facebook.